If you have glaucoma, you may experience random blind spots in your vision. You may get regular bouts of sharp pain in the eyes or severe headaches. The condition is caused by excess pressure inside the eyes, and it can cause damage to the optic nerve. Diabetes increases your risk of glaucoma.
Understanding Glaucoma
Glaucoma is among the top causative factors for blindness in people aged 60 and above. It damages the optic nerve, which plays indomitable roles in vision and ophthalmic wellness.
When glaucoma is not detected early or if it goes untreated, the severe damage it causes to the optic nerve can cause blindness. There is still plenty left to learn regarding this eye condition. What we know now is that glaucoma damages the optic nerve by causing a build-up of aqueous humor and increases pressure in the eye.
Diabetes increases your risk of developing glaucoma. You may slowly lose vision or start to see bright colored rings when looking at lights. Treatment approaches for glaucoma include prescription eye-drops, which eye pressure, and surgery for advanced cases.
Aqueous Humor and Intraocular Pressure
The eyes continuously produce a colorless fluid that occupies the space inside the eye. This is the aqueous humor. New fluid often flows in and replaces older fluid, which leaves the eye through drainage channels.
If there is a blockage to this flow, intraocular pressure—the pressure inside the eye—rises. Excessive IOP damages the optic nerve.
Types of Glaucoma
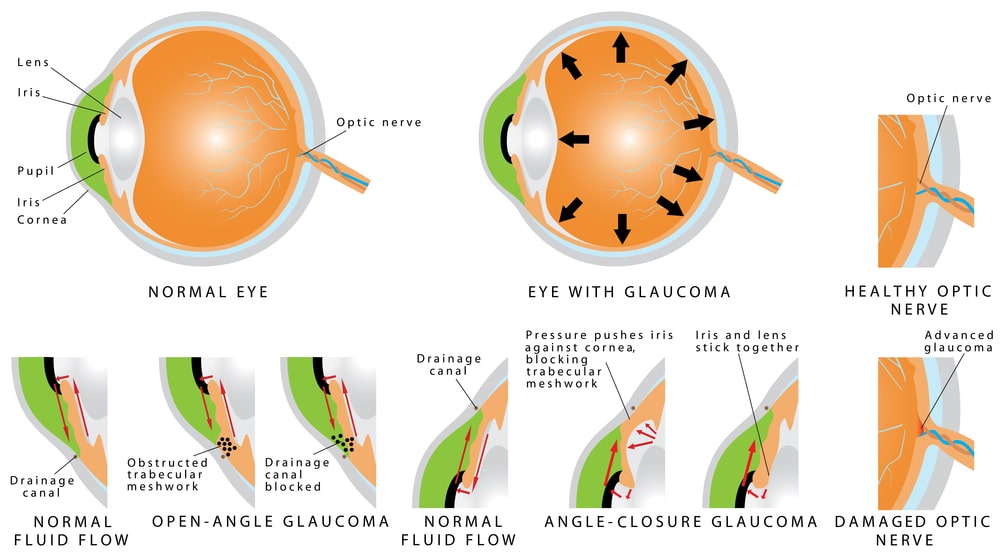
There are two types of glaucoma. One happens fast, and the other occurs over a long period.
Closed-angle glaucoma
This happens suddenly, and it is a medical emergency. The iris pushes forwards and reduces the drainage angle between the cornea and the iris. This blocks the aqueous humor from flowing out and causes excessive pressure inside the eye.
Closed-angle glaucoma is not related to diabetes.
Open-angle glaucoma
This happens gradually, and patients may show no symptoms. The drainage space between the cornea and the iris stays open, but the drainage channels are partially blocked. The pressure inside the eye builds slowly. Vision loss occurs gradually.
There is a relationship between diabetes and open-angular glaucoma.
Diabetes and glaucoma
The most direct connection between diabetes and glaucoma is diabetic retinopathy. The latter is an eye complication caused by diabetes. It damages the capillaries at the back of the eye.
Diabetic retinopathy elevates the risk of glaucoma. Close to 8 million Americans aged 40 and older have diabetic retinopathy. Risk factors for the condition include high blood sugar levels, age, and high blood pressure.
Fluctuations in blood glucose level can weaken and damage blood vessels in the retina. This impacts the circulation of the fluid in the eye, leading to a buildup of pressure.
Following the damage, the retina may make new abnormal blood vessels. When the new abnormal blood vessels grow on the iris, the condition is called neurovascular glaucoma. The blood vessels block the eye’s drainage channels, leading to excessive pressure inside the eye.
Also, high blood pressure caused by diabetes can directly lead to glaucoma. Research shows that high blood pressure causes the eyes to make more fibronectin. The latter is a glycoprotein made to protect the eye’s cells—this protein, however, can block your eye’s drainage system.
Diabetes glaucoma symptoms
In all cases of glaucoma, whether diabetes is involved or not, the condition has very few symptoms. Notably, open angular glaucoma causes gradual vision loss. You may never realize until it’s too late. Regular eye checkup is strongly advisable.
For those that show symptoms, glaucoma may manifest in the form of:
- Blind spots and tunnel vision for open angular glaucoma
- Intense sharp pain in the eye, severe headache, blurry vision, and eye redness for closed-angle glaucoma
- Vision loss, red eyes, and eye pain for neurovascular glaucoma
Diagnosis and treatment
The CDC stresses that individuals with diabetes should get a dilated eye exam at least once every year. This exam helps the eye specialist check the health condition of the back of the eye and identify nerve damage issues.
Diagnosis may also entail measuring eye pressure in the eyes and measuring the width of the cornea.
Treatment approaches for glaucoma include prescription eye drops. If that proves ineffective, the ophthalmologist may prescribe medication or surgery.
Types of surgeries for glaucoma include:
- Drainage tube implants to help remove the fluid in the eye
- Laser therapy to unclog blocked drainage channels in the eye
- Removal of damaged parts of the eye drainage system
How else does diabetes risk eye health?
High blood pressure and prolonged high blood sugar levels can lead to eye conditions such as cataracts and macular edema.
Cataracts: If you have diabetes, cataracts may come way earlier before your 60th birthday. It is believed that the presence of high glucose amounts in the blood causes deposits to accumulate in the lens of the eye.
Diabetic macular edema: DME causes fluid buildup in the back of the eye—the macula. The macula is the core of the retina that enables us to see. It has light-sensitive cells. Damage to the macula from the fluid build-up can cause vision loss.
If you have diabetes, protect your eye health by reducing blood sugar levels (through diabetes medication), regular physical exercise, and getting an eye dilation exam every year.